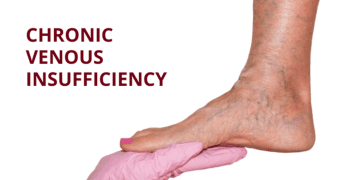
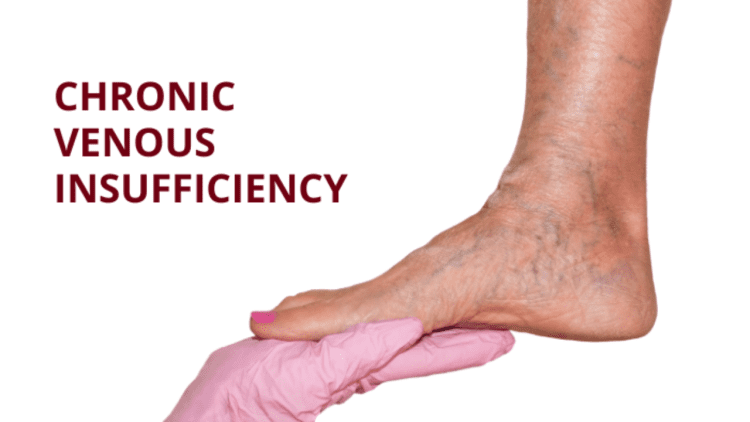
Introduction: What Is Chronic Venous Insufficiency?
Chronic Venous Insufficiency (CVI) is a vascular condition that affects the veins in the legs, impairing their ability to return blood to the heart.
Normally, veins contain one-way valves that prevent blood from flowing backward.
In CVI, these valves become damaged or weakened, causing blood to pool in the lower limbs.
This leads to increased venous pressure, swelling, skin changes, and in severe cases, painful ulcers.
CVI is not immediately life-threatening, but it can significantly impact quality of life.
It’s a progressive condition that affects millions worldwide, especially older adults, women, and individuals with a history of blood clots or varicose veins.

Causes of Chronic Venous Insufficiency
CVI can result from a variety of structural and functional issues in the veins. The primary causes include:
1. Valve Malfunction
Congenital: Some individuals are born with defective or absent venous valves.
Primary: Veins may enlarge or stretch, preventing valves from closing properly.
Secondary: Damage from other conditions, such as deep vein thrombosis (DVT), can scar valves and impair function.
2. Deep Vein Thrombosis (DVT)
Blood clots in deep veins can block blood flow and damage valves, leading to long-term insufficiency.
3. Prolonged Standing or Sitting
Occupational habits that involve long periods of immobility can increase venous pressure and strain valves.
4. Obesity and Pregnancy
Excess weight and increased blood volume during pregnancy place additional pressure on leg veins.
5. Smoking and Aging
Smoking damages vein walls and valves, while aging naturally weakens vascular structures.
Risk Factors
Several factors increase the likelihood of developing CVI:
• Age over 50
• Female gender (due to hormonal changes and pregnancy)
• Family history of vein disorders
• Sedentary lifestyle
• History of leg injury or surgery
• Smoking
• Obesity
Symptoms of Chronic Venous Insufficiency
CVI symptoms often begin subtly and worsen over time. Common signs include:
1. Swelling in the legs or ankles (especially after standing)
2. Aching or heaviness in the legs
3. Cramping or burning sensations
4. Itchy or flaky skin
5. Discolored skin, often reddish-brown near the ankles
6. Varicose veins
7. Leg ulcers that are slow to heal
8. Leathery or hardened skin texture
9. Restless legs syndrome or painful spasms
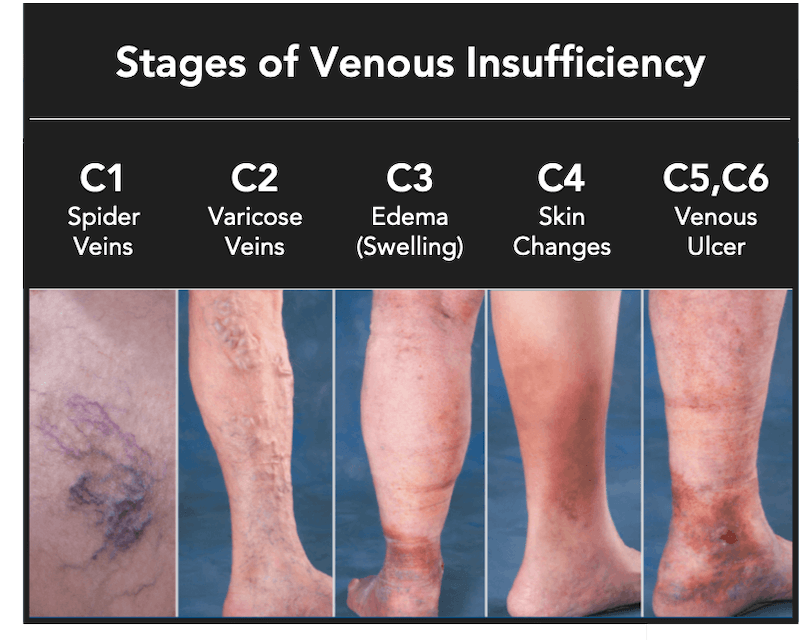
Stages of CVI
Doctors classify CVI using a staging system from 0 to 6:
| Stage | Description |
| 0 | No visible signs, but symptoms like achy legs may be present |
| 1 | Spider veins or visible blood vessels |
| 2 | Varicose veins at least 3 mm wide |
| 3 | Swelling without skin changes |
| 4 | Skin discoloration or texture changes |
| 5 | Healed ulcers |
| 6 | Active ulcers |
Diagnosis typically begins at Stage 3, when swelling becomes clinically evident.
Diagnosis
CVI is diagnosed through a combination of:
Physical examination: Checking for swelling, skin changes, and varicose veins
Duplex ultrasound: Evaluates blood flow and valve function
Venogram or MRI: Used in complex cases to assess vein structure and rule out other conditions
Treatment Options
Treatment for Chronic Venous Insufficiency focuses on improving blood flow, reducing symptoms, and preventing complications.
Options range from conservative measures to surgical interventions.
Lifestyle Changes
Leg elevation: Reduces pressure and promotes venous return
Exercise: Walking and calf-strengthening exercises improve circulation
Weight management: Reduces strain on veins
Avoid prolonged sitting or standing: Encourages blood flow
Compression Therapy
Compression stockings are the first line of treatment
Graduated compression helps push blood upward
Prescription-strength stockings may be needed for advanced cases
Medications
Aspirin: Helps heal ulcers
Diuretics: Used if swelling is linked to heart or kidney issues
Blood thinners: Prevent clot formation in high-risk patients
Minimally Invasive Procedures
Endovenous laser ablation (EVLA) or radiofrequency ablation (RFA): Heat closes off damaged veins
Sclerotherapy: Chemical injection collapses faulty veins
Microincision phlebectomy: Removes damaged veins through small punctures
Surgical Options
Vein ligation and stripping: Ties off or removes severely damaged veins
Vein repair or transplant: Restores function in select cases
Vein bypass: Reroutes blood flow in extreme cases
Living with CVI
Managing CVI requires ongoing care and lifestyle adjustments:
Daily use of compression garments
Regular movement and stretching
Heart-healthy diet: Low in sodium, rich in fiber and antioxidants
Hydration: Supports circulation
Avoid smoking: Preserves vein health
Complications
If left untreated, CVI can lead to:
Venous ulcers: Painful, slow-healing wounds prone to infection
Cellulitis: Skin infection that can spread
Deep vein thrombosis (DVT): Increased risk due to blood pooling
Pulmonary embolism: Life-threatening if clots travel to the lungs
Prevention
While not all cases of CVI can be prevented, you can reduce your risk by:
Maintaining a healthy weight
Exercising regularly
Avoiding prolonged immobility
Wearing compression stockings if recommended
Managing blood pressure and avoiding smoking
Conclusion: Managing Chronic Venous Insufficiency
Chronic Venous Insufficiency is a common yet underrecognized condition that can cause discomfort, skin damage, and serious complications if ignored.
Fortunately, with early diagnosis and a combination of lifestyle changes, compression therapy, and medical interventions, CVI can be effectively managed.
Whether you’re experiencing mild symptoms or dealing with advanced stages, proactive care and consultation with a vascular specialist can help restore comfort and prevent progression.
CVI may be chronic, but it doesn’t have to control your life.
Frequently Asked Questions
Q. What is Chronic Venous Insufficiency (CVI)?
CVI is a condition where the veins in your legs are unable to efficiently return blood to the heart due to damaged or weakened valves. This causes blood to pool in the lower limbs, leading to swelling, discomfort, and skin changes.
Q. What causes Chronic Venous Insufficiency?
CVI is often caused by valve damage due to aging, deep vein thrombosis (DVT), prolonged standing or sitting, obesity, pregnancy, or a sedentary lifestyle. These factors increase pressure in the leg veins, weakening their ability to function properly.
Q. What are the symptoms of CVI?
Common symptoms include:
Swelling in the legs or ankles
Achy or heavy legs
Cramping, especially at night
Itchy or flaky skin
Skin discoloration (reddish-brown)
Varicose veins
Slow-healing leg ulcers
Q. How is CVI diagnosed?
Diagnosis typically involves a physical exam and a duplex ultrasound, which assesses blood flow and valve function. In some cases, additional imaging like MRI or CT scans may be used to rule out other conditions.
Q. Is CVI a serious health condition?
While CVI is not usually life-threatening, it can be painful and disabling if left untreated. It may lead to complications like venous ulcers, skin infections (cellulitis), and increased risk of blood clots.
Q. How common is Chronic Venous Insufficiency?
CVI affects about 1 in 20 adults, with approximately 150,000 new cases diagnosed annually in the U.S. It is more common in people over 50 and those with a history of varicose veins or DVT.
Q. Can CVI be cured or reversed?
Chronic Venous Insufficiency cannot be fully cured or reversed, but its symptoms and progression can be managed effectively through lifestyle changes, compression therapy, medications, and minimally invasive procedures.
Q. What treatments are available for CVI?
Treatment options include:
Compression stockings
Leg elevation
Exercise and weight management
Medications like blood thinners or aspirin
Procedures such as sclerotherapy, endovenous ablation, or vein stripping in severe cases.
Q. How can I prevent Chronic Venous Insufficiency?
Prevention strategies include:
Regular physical activity
Maintaining a healthy weight
Avoiding prolonged sitting or standing
Wearing compression garments if recommended
Not smoking and following a heart-healthy diet.